About The Project
The initial aim of this project was to address the response times to hospital patient call lights, which could represent a significant safety concern. This could be attributed to factors such as a lack of clarity in the call light's purpose, misuse of the system, and a high volume of calls. The current patient call light experience involves pressing a button and waiting, which poses challenges when patients have varying needs, from simple requests like water to urgent situations. To enhance both the hospital patient experience and operational efficiency, a redesigned patient call light system was deemed to be necessary.
However, as I progressed through this project my scope narrowed from redesigning the hospital patient call light to enhancing the overall patient experience. This transition occurred when I encountered the Hillrom Centrella Ecosystem and began uncovering various stakeholder needs. This document serves as a narrative of my journey throughout this project, delving into key insights from hospitals to address patient-nurse interaction within the medical space.
Exploring The Current Call Light Ecosystem
How does the current call light system work?
Methods
Secondary Research | Structured Stakeholder Interviews
Output
User Flow Creation
To locate existing call light systems and understand how they work I did some desk research into a current system. I also interviewed three nurses, one respirataroy therapist, and one med-surge patient. During the interviews I asked about which system they use or used for patient-nurse interaction (call light) and their overall experience using these devices. I documented two different call light ecosystems: The Responder 5 and The Hilrom Centrella Ecosystems.
When I first began this project, I assumed that the call light systems leveraged by the hospitals were much more simplistic. I assumed that there was one call light button available to a patient, after clicked a white dome light would appear above the patients door signifying the patient needs assistance.
The Responder 5
The Rauland Responder 5 call light system was the leading patient-nurse interaction device prior to the Hilrom Centrella Ecosystem. This was the first system I discovered via stakeholder interviews and is still leveraged by many hospitals within the United States. Below outlines how a patient and nurse interact via this system.

Figure 2 - Responder 5 Patient Remote displaying activation affordances.
Hilrom Centrella
While talking to a hospital staff worker, respiratory therapist, they pointed out to me a new call light patient-nurse interaction system they had recently been implemented into their hospital. This system was called Hilrom Centrella. The Centrella system features a wide range of devices that all work together. To my understanding, this is the newest system available for medical facilities.
Below is a user flow as to how the Hilrom Centrella ecosystem works.
Figure 3 - User Flow displaying a patient-nurse interaction leveraging the Hilrom Centrella Ecosystem
While researching the Hilrom Centrella, I noticed a device apart of the ecosystem that attempts to improve the hospital patient experience. This device is called the Experience Pod (figure 4).
Figure 4 - The Experience Pod
Device Affordances
Holds and charges patient's device (ie: Smartphone, Tablet, etc.
Swivels to view front and back
Always in reach of patient
Adjusts bed position
Activate Call Light
TV remote
~$2,000 per device
Optional add on device for ecosystem, not required for ecosytem to work. Without this device patients will use a traditional remote shown on right in figure 4.
Discovery Result
Uncovering these devices informed me of the ecosystem that I am currently designing in. It assisted me in understanding the potential flows that both the patient and hospital staff progress through in order to achieve a call light notification response. This research corrected my pre conceived assumptions about my space.
During the time I researched these devices, I also located pain-points in the patient-nurse interaction as well as the hospital-call light experience, which will be covered in the next section of this document.
Exploring Patient-Nurse Interaction
What do patients and nureses dislike about the current system?
Methods
Secondary Research | Structured Stakeholder Interviews | Experience Mapping
To locate painpoints in the current call light and patient-nurse interaction ecosystems, I talked to and researched a variety of stakeholders within the medical field environment.
My structured interviewed included two nurses, a CNA, and one hospital patient. I also had unstructured casual conversations with medical staff.
I browsed Reddit experiences of both nurses and patients regarding patient-nurse interaction and patient hospital experience.
Pain Points
Nurse
Patient
Call Light Ambiguity
(Interviews)
Accidental Presses
(Interviews)
Call Light Abuse
(Interviews, Reddit)
Alarm Fatigue
(Interviews, Reddit)
Interruption Exhaustion
(Interviews, Reddit)
Call Light Location
(Interviews)
The Remote
(Interviews)
Overview of found patient painpoints within the patient-nurse call light interaction.
Use Cases
(Interviews, Reddit)
Need Water
Want Food/When is food coming?
Needs help with TV
"I'm in pain"
Wants more medication
"When is my next medication dose?"
Questions about paperwork
Questions about hospital record
"Am I ready to leave?"
"When is therapy?"
"What am I doing in Therapy?"
"I'm Nauseous."
"I need help making a phone call."
Needs to go to bathroom
"I just wanted to say hi."
Pillow Adjustments
Overview of call light use cases presented to my attention.
Highlights
(Interviews)
Nurses will answer call lights as they walk by.
Priority given to those who have been waiting the longest.
"Independent patients are best"- Nurse
Nurses get notifications via a Vincero like device, lights above the door, and at the nurses station.
The most modern hospitals leverage the Centrella Ecosystem.
Patient MyChart access is a desired feature from nurses.
Overview of call light highlights presented to my attention.
Patient Satisfaction
Why is Patient Satisfaction Important?
Methods
Secondary Research
Hospitals are required to participate in a publicly recorded survey that measures various standards of patient satisfaction. These surveys are handed out to a random number of patients at every U.S. hospital consisting of 29 questions. These surveys measure the communications with nurses/doctors, responsiveness of staff, cleanliness/quietness, medicine communication, discharge info, and overall hospital rating. They must also state whether they recommend a hospital.
Three Goals:
Produce data about patients' perspectives of care that allow objective and meaningful comparisons of hospitals on topics that are important to consumers.
Public reporting of the survey results create new incentives for hospitals to improve quality of care.
Public Reporting serves to enhance accountability in healthcare by increasing transparency of the quality of hospital care provided in return for pubic investment.
User Research Result
I talked to hospital stakeholders (nurses, patients, staff) throughout the entire duration of this project. Some of these conversations were structured as more professional interviews, while others were unstructured casual conversations.
I categorized the data I received from these stakeholders into 7 categorized painpoints, highlights, and justifications as to why people leverage the call light. I located a survey pointed out to me by one of my stakeholders which encourages hospitals to bring a good experience to their patients.
This data assisted me in moving forward in my problem space. It enabled me to begin crafting an experience map and user flow of painpoints, highlights, and experiences which will be covered next. It also uncovered potential value to improve the patient experience.
Mapping the Data
What needs to be improved within the current hospital call light enviroment?
Methods
User Flow Creation | Affinity Diagram | Experience Map Matrix
After locating stakeholder pain-points and researching the current environment, I needed to begin a deeper analysis. To achieve this, I mapped out a user flow (figure 5) to guide my creation of an experience map matrix diagram. I did this to locate the best opportunities for possible improvement.
User Flow of Stakeholder Painpoints
Before I began crafting an experience map matrix, I wanted to create a flow mapping out how my stakeholders interact with the call light environment, leveraging all the data I have collected to this point. I then used this flow to create my experience map matrix to identify design opportunities.
User Flow overview of potential call light scenarios with identified user painpoints highlighted.
Potential Design Opportunities
I created an experience map to uncover all the opportunities that I can design for using the data I have collected. Below are all the found opportunities I identified from my experience map.
Narrowing my Scope
I learned that the call light may not be the actual problem leading to upset stakeholders. I uncovered that solely improving a patient's hospital experience may work better toward creating a better nurse-patient interaction environment. I decided to narrow my scope to "Improving the Patient Hospital Experience." I did this to focus on one user, the patient, and to assist hospital patient survey results. Many of my found design opportunities also involved the patient over the staff. Next I began designing for this goal.
Improving the Patient Experience
How can we improve the Patient Hospital Experience?
Methods
Lofi Concept
For my design, I decided to work within one of the two existing ecosystems that I located during this project. I did this to keep my result feasible and to ensure easy implementation. I decided to work off of the Hilrom Centrella Ecosystem.
While researching the Hilrom Centrella Ecosystem, I encountered a device called the Experience Pod. This pod was an exisiting example of an attempt to improve the patient hospital experience. The main concern with this existing device was its lack of functionality. It did not do much for the patient, only holding the patients device and making the bed remote easy to access.
I expanded upon the Hilrom Centrella Experience Pod device via a low fidelity mockup to communicate and test my concept to my stakeholders.
Figure 6 - Experience Pod Plus - Lofi of Patient Overview
The updated Experience Pod Plus will have both a digital and physcial interface for the user to interact with. The first interface shown (figure 6) is the home page for the device. The home page or overview page is used to communicate to the patient their current state during a hospital stay at a glance.
This page is used to replace the whiteboard in current hosptial patient rooms with a digital system. It provides the patient with information to increase independence and decrease calling the nurse for such information.
Figure 7 - Experience Pod Plus - Lofi ofMyChart Access *MyChart page never designed out, features placeholder image that I do not own*
The second page on this new Experience Pod Plus Device gives the hospital patient access to MyChart (figure 7). MyChart is a hospital patient portal displaying medical records and information to a patient.
This page was added per the request of a nurse that I spoke to. She mentioned how her hospital used to give patients a tablet to get access to MyChart, but the hospital halted this feature for the patients. She was unsure why the hospital decided to halt this feature, but wished for it to be brought back to the patients.
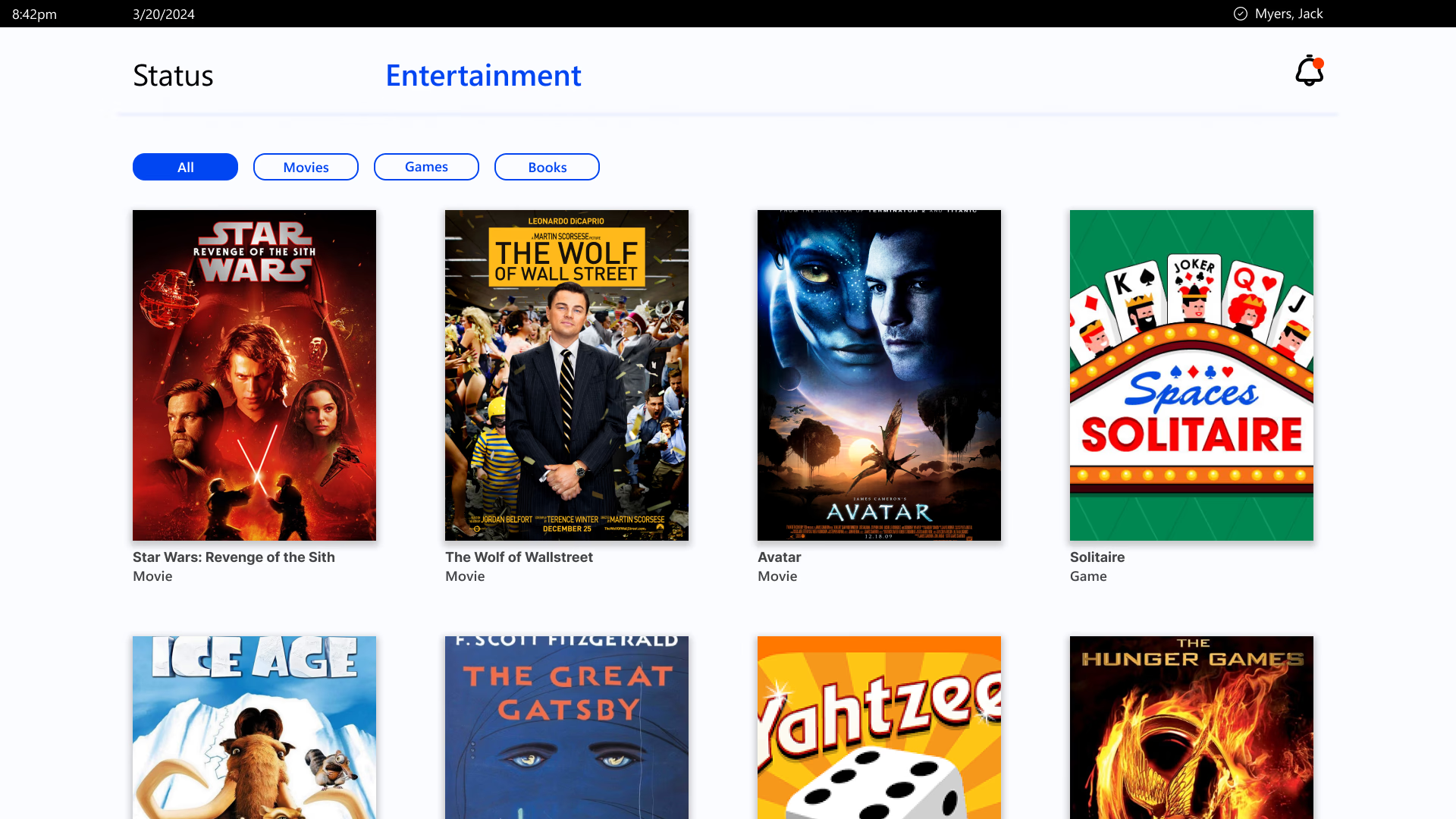
Figure 8 - Experience Pod Plus - Lofi of Patient Entertainment
The third page on the new Experience Pod Plus was the entertainment page. On this page the patient can select from a library containing an assortment of movies, games, and books to keep the patient entertained during their hospital stay. This feature would work similar to how airlines give passengers access to a similar feature.
While visiting a hopsital patient for one of my interviews, the patient explained to me how bored they were. They explained that not much was on TV, and that she would "love to watch a movie." Nurses also informed me that bored patients can cause trouble to the staff. These concerns influenced this page.
Figure 9 - Experience Pod Plus - Lofi of Enhanced Call Light Feature
The updated Experience Pod Plus will have an enhanced call light feature. This feature would give the hospital the ability to rotate and customize call light options to cater towards a specific patient. For example, if the patient has a catheter in, they will have a call light specific to the catheter. Upon activation of the call light a audio signifier would alert the patient that the call light has been activated and the interface would be surrounded by a gradient shown in figure 9.
This page is used to communicate to better communicate patient needs to hosptal staff.
Testing the Concept
Is this concept feasible for hospitals?
Methods
Unscripted Concept Testing
Due to several constraints within this project I was unable to do formal concept testing with my design. Instead, I showed this concept to several hospital staff and regular people. I asked the hospital staff if they would appreciate patients having a device like this, if there was any information the patient should not have access to, and if this device was logistically feasible.
I also talked to regular people to see if they would appreciate a device like this if they were in a hospital. I categorized this user group as patients for the results of this test.
I divided the information brought to me in several categories:
Overview Page:
Pros:
Both groups appreciate info displayed on this page.
According to nurses, it is ok for the patients to have easy access to this info.
Both groups feel this would improve quality of life during a patient stay.
Cons:
Nurses wonder who would keep the info up to date on this page.
MyChart:
Pros:
Patients appreciated this page.
Cons:
Nurses explained that the patient may see test results before staff have explained the results, which will prompt them to call for assistance before the staff are ready to communicate the test results.
Entertainment:
Pros:
Highly valued by both groups as current cable TV is outdated.
Cons:
N/A
Call Light:
Pros:
Staff appreciate the customizability
Cons:
May be harder for patients to access as it is on its own separate page
Who will cycle in new buttons for the patient?
How will this effect the current call light environment within Hilrom Centrella?
How will the different needs be communicated to staff?
I turned my wireframes into a higher fidelity iteration to better communicate my ideas to stakeholders, and to enable my designs to be properly tested in the future.
The Experience Pod (current)
Figure 10 - Hilrom Centrella Experience Pod
The Experience Pod Plus (new)

Figure 11 - Hilrom Centrella Experience Pod Plus
The new Hilrom Centrella Experience Pod will use a similar design to the original, leveraging the flip mechanism to reveal the TV remote. The main difference with the Experience Pod Plus is the addition of a digital interface on the pod. The new pod is outfitted with audio speakers and microphone for communication with staff.
There is also a new "do not disturb" button located on the pod. This button will illuminate the dome light above the patients door to "purple" which signifies to passing staff to shut the patients door, and only bother the patient if needed.
All buttons on the Experience Pod Plus are tactile and easier to press, excluding the digital interface.
Hover for quotes
Patient Quote
Staff Quote
Status "homepage" HiFi
Opportunities Addressed
How might we make patients more independent?
How might we prevent call light exhaustion?
Call light activation requests:
"When is my next therapy session?"
"What time is my therapy?"
"Am I ready to leave?"
"When is my next pain med dose?"
How might we ease patient anxiety?
"I get anxious of my health state."
How might we limit staff interruption exhaustion?
Update Patient Pain Levels
Out of date Medical Board
Old vs New Flow
Patient Needs Info -> Reads Whiteboard (hasn't been updated)
Patient Needs Info -> Activates Call Light and Waits
Patient Needs Info -> Looks at Experience Pod Plus
Notifications HiFi
Opportunities Addressed
How might we ease patient anxiety?
"Is a nurse coming?"
How might we ensure the patient that they have been heard?
Old vs New Flow
Patient wonders if nurse is coming -> Is unsure
Patient Wonders if Nurse is coming -> Checks notifications
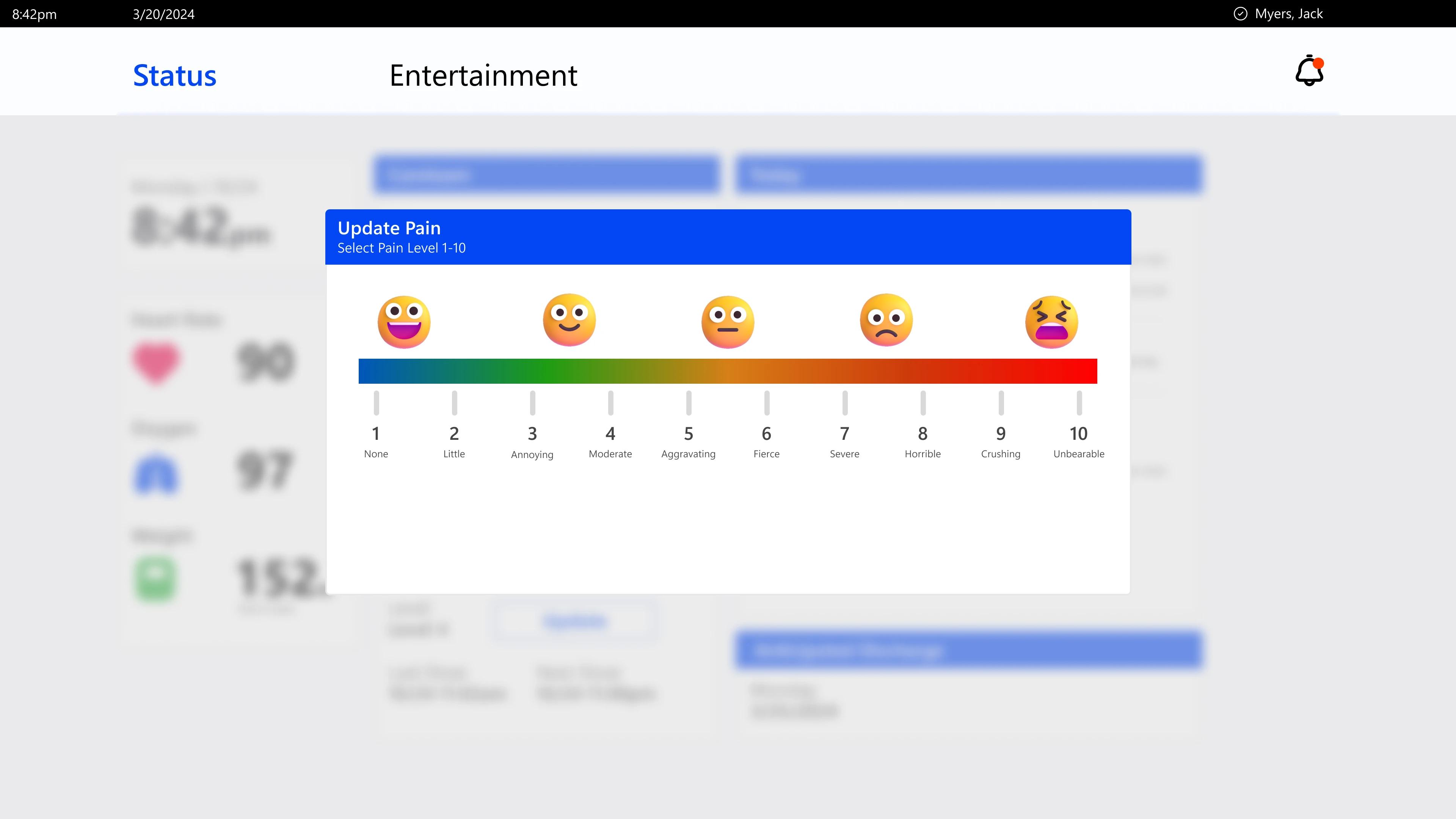
Pain Level Update HiFi
Opportunities Addressed
How might we increase Patient Independence
How might we automate some staff tasks?
Old vs New Flow
Nurse must assess Patient pain levels -> Visits Patient
Nurse must assess Patient pain levels -> Reads Experience Pod Plus
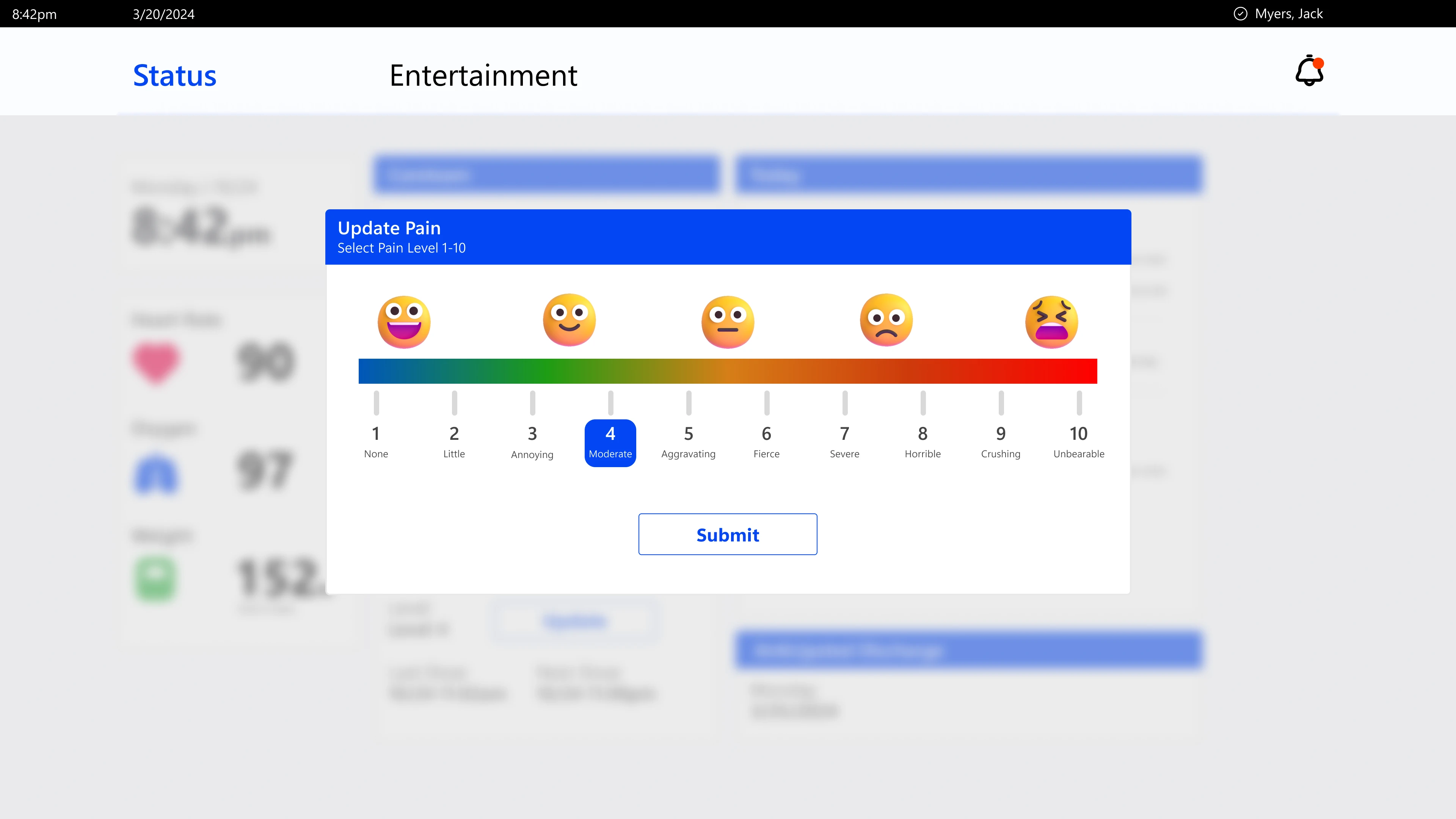
Entertainment HiFi
Opportunities Addressed
How might we entertain patients?
"I would love to watch a movie."
"I feel like I am in jail."
"I like to keep the door open to watch people walk by."
"Patients seem to abuse the call light when they are bored."
Old vs New Flow
Patient is bored -> Watches cable TV
Patient is bored -> Looks out window/door
Patient is bored -> Bothers staff
Patient is bored -> Accesses a variety of modern entertainment options
Call Light Options HiFi
Opportunities Addressed
How might we make the call light more accessible?
Currently within the Hilrom Centrella Experience, patients must talk to the staff via the staff console to explain call light requests. What if the patient can not talk?
Requests communicated to staff via text to speech through staff console.
Old vs New Flow
Patient needs staff -> Patient can not talk to staff -> Patient needs unmet
Patient needs staff -> Patient can not talk to staff -> Enters input on Experience Pod Plus
Bonus Features
Features Requested by Staff during Concept Testing
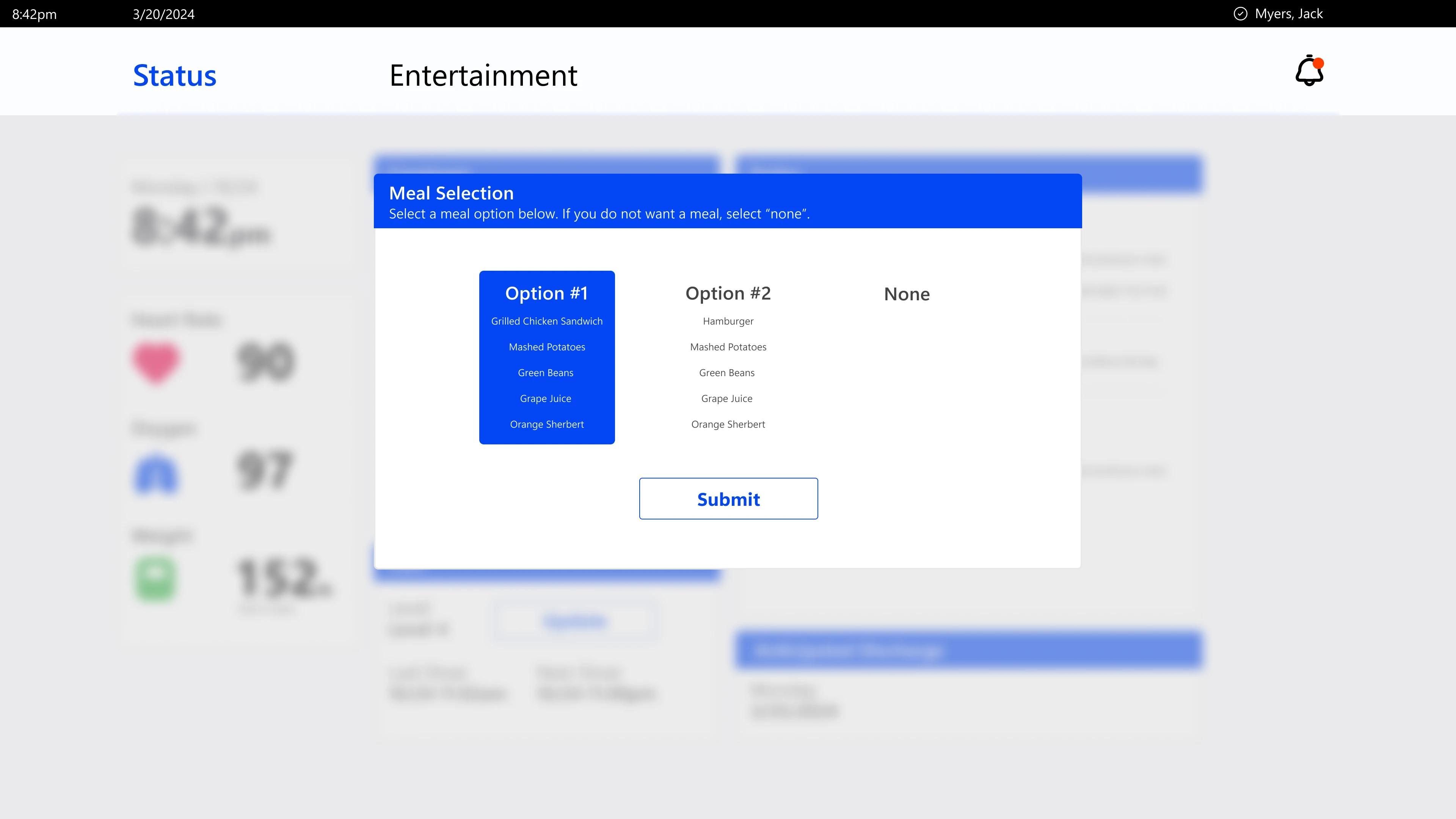
Meal Order HiFi
Opportunities Addressed
How might we increase Patient Independence
How might we automate some staff tasks?
Old vs New Flow
Nurse must gather meal order -> Visits Patient -> Collects meal order -> Looses meal order -> Revisits patient
Nurse must gather meal order -> Sends message to Experience Pod Plus
Doctor Video Call
Opportunities Addressed
How might we automate some staff tasks?
Old vs New Flow
Doctor Wants a meeting with patient -> Visits Patient
Doctor Wants a meeting with patient -> Staff brings patient IPad
Doctor Wants a meeting with patient -> Calls patient via the Experience Pod Plus
The Value
Hypothesized Value *untested*
Why would hospitals want to invest in this device?
Decreases call light activation, giving more time to nurses and other hospital staff
By giving access to information that the patient would previously need staff for
Increases Hospital Patient Independence
By giving the patient up to date information regarding their hospital status
Increases Patient Hospital Stay Satisfaction to boost NHCS survey results, granting public funding
Patient satisfaction is increased by the access to modern entertainment, reduced patient boredom
Information regarding their hospital stay to increase transparency
Increased Hospital Staff Communication
Staff can see care team of a patient via the device
Staff can monitor a patients pain levels and recovery over a wider range of time
Enhanced Accessibility
"Write in" option for call light
Limitations
Insufficient access to hospital space, leading to assumptions regarding the users and space that can not be tested
Large design space with lots of data. Limited time and resources (team of one).
Hospitals use a variety of technologies from various ecosystems, for this project I had to assume that a hospital used the Centrella Ecosystem in its desired use case.
Giving users more information access can be hypothesized to increase call light activation.
This project is not fully completed, more logistical aspects must be thought about in order to make this product feasible. A second software must be designed in order for staff to manage the Experience Pod Plus systems.
If more time was given for this project, I would create a scenario based wizard of oz testing to assess if this product improves my found design opportunities.
Reflection
I dove into this user-centered project with a more direct approach, meaning that I would try to solve a direct problem: Redesign the call light environment to improve the experience for both patients and nurses. I quickly learned that this is a very heavy task to complete as a team of one during a one semester college class. I was unfamiliar with my problem space at the start of this project, leading to the project being very broad as I had a lot to learn.
I learned that the call light may not be the actual problem leading to upset stakeholders. I uncovered that solely improving a patient's hospital experience may work better toward creating a better nurse-patient interaction environment. This enabled me to practice a change in scope and challenging assumptions. Being a team of one attempting to tackle such a broad problem, I learned more in this project than any of my previous projects.
If I could talk to myself at the begining of this project, I would have said to be prepared to think holistically in the hospital environment and not stress about creating something that will improve the experience for everyone.